Abstract
Introduction: The NHLBI MDS Natural History Study (NCT02775383) is an ongoing prospective cohort study conducted across 144 sites in the U.S. and Israel intended to establish a data and biospecimen repository to advance the understanding of MDS. In response to the COVID-19 pandemic, the study also collected data on COVID-19 infection and management. Here, we report a summary of COVID-19 outcomes from participants in this study and the impact of the pandemic on study operations.
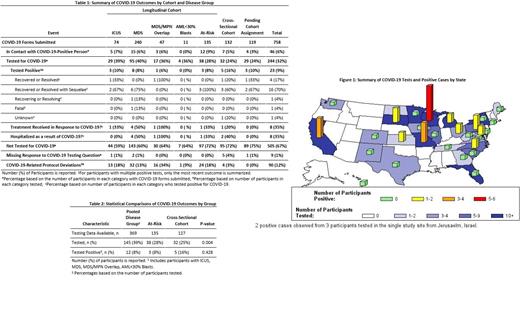
Methods: This prospective cohort study initiated in June, 2016 is enrolling patients (pts) undergoing diagnostic work up for suspected or newly diagnosed MDS or MDS/myeloproliferative neoplasms (MPNs) in the setting of cytopenia. Study enrollment was paused from Mar. 27, 2020 to May 18, 2020 due to COVID-19. Previously untreated pts underwent a bone marrow assessment with a centralized histopathology review at enrollment for assignment to a longitudinal cohort (MDS, MDS/MPN overlap, idiopathic cytopenia of undetermined significance (ICUS), acute myeloid leukemia (AML) with <30% blasts, or "At-Risk" (pts with sub-threshold dysplasia, select karyotype, or select genetic mutations) for follow-up every six months; or a cross-sectional cohort (other cytopenia or cancers) with no further follow-up. COVID-19 outcomes, including tests, status, hospitalizations and treatments for COVID-19, were collected for all eligible pts. Protocol deviations related to COVID-19 were also collected. Fisher's exact test was used for comparing the proportions of pts tested or positive between groups.
Results: Of 758 eligible pts with available COVID-19 data, 507 (67%) were assigned to the longitudinal cohort and 251 (33%) to the cross-sectional cohort or are pending assignment. Among longitudinal pts, 74 (15%) had ICUS, 240 (47%) MDS, 47 (9%) MDS/MPN overlap, 11 (2%) AML with <30% blasts, and 135 (27%) At-Risk for MDS. The median age over all pts was 72 years (range=21-95) and 66% were male, 92% White, 4% Black, 2% Asian, and 2% other.
Among 244 pts (32%) tested for COVID-19 (Table 1), 23 (9%) were positive. Twelve (>50% of the positive pts) were in Wisconsin, California (CA), and Missouri (Figure 1), with 8 identified from Sep. to Dec. 2020, which overlaps with third waves of COVID-19 reported in CA and in the Midwest. Tests from 17 (74%) of the 23 pts were based on a polymerase chain reaction (PCR) assay. The proportion of pts positive were similar between pooled disease (ICUS, MDS, MDS/MPN, AML <30%), At-Risk, and cross-sectional groups (8%, 8%, 16%, respectively; Table 2) but the proportions tested differed significantly (39%, 28%, and 25%, respectively, p=0.004).
Among all positive pts, 21 (91%) are recovering or have recovered (16 with sequelae), 1 (4%) died, and 1 outcome is unknown (Table 1). The one participant who died had MDS with excess blasts-1 (MDS-EB1, 5-9% blasts). Eight pts (35% of positive pts) required hospitalization (median duration of 7 days (range=2-17)) or treatment (tx) in response to COVID-19, 7 of whom required both. In the 8 pts who required tx for COVID-19, 4 reported Remdesivir-use, 3 of whom were diagnosed with MDS or MDS/MPN overlap.
The study monthly accrual rates were similar when compared pre- vs. post-study pause (23 vs. 22 pts, respectively) but the rate of missed follow-up visits increased from 5% to 11% post-pause. About half (49%) of the 144 COVID-19-related study deviations occurred during the months the study was paused.
Conclusions: In this analysis of 758 pts with MDS and related conditions, the largest reported for these diagnoses, the COVID-19 mortality rate (13%) in MDS was lower than has been reported in a smaller (n=61) case study (39%, Feld et al Blood 2020) but is similar to the rates for MDS observed annually each year prior to study pause (range=11-19%) and to the rate reported in a larger (n=2186) observational study of cancer patients (16%, Rivera et al Cancer Discov 2020). Infection rates were similar across disease groups. The pandemic also resulted in substantial study-specific challenges, including increased rate of deviations, the study being paused, and difficulty sourcing material for biospecimen processing. Data on vaccine efficacy and rates of pts with long-haul symptoms post-COVID may be of interest in future work.
Padron: BMS: Research Funding; Kura: Research Funding; Taiho: Honoraria; Stemline: Honoraria; Blueprint: Honoraria; Incyte: Research Funding. Komrokji: Novartis: Honoraria; Geron: Honoraria; Acceleron: Honoraria; Agios: Honoraria, Speakers Bureau; Abbvie: Honoraria, Speakers Bureau; JAZZ: Honoraria, Speakers Bureau; BMS: Honoraria, Speakers Bureau. Saber: Govt. COI: Other. Al Baghdadi: Bristol-Myers Squibb: Current holder of individual stocks in a privately-held company, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Current holder of individual stocks in a privately-held company; Epizyme: Current holder of individual stocks in a privately-held company; Heron Therapeutics: Current holder of individual stocks in a privately-held company; Morphosys: Membership on an entity's Board of Directors or advisory committees; Karyopharm: Membership on an entity's Board of Directors or advisory committees; Cardinal Health: Membership on an entity's Board of Directors or advisory committees. DeZern: Taiho: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees. Sekeres: Novartis: Membership on an entity's Board of Directors or advisory committees; Takeda/Millenium: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal